Centurion offers a dental insurance plan through Delta Dental of Virginia.
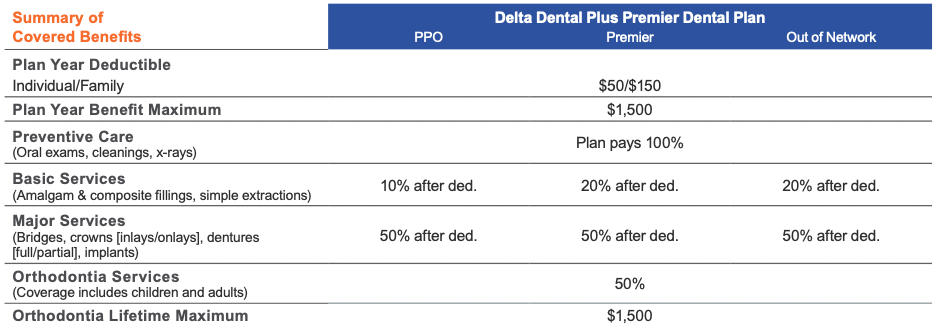
The dental plan provides in- and out-of-network benefits, allowing you the freedom to choose any dentist. The amount you pay varies based on whether you see a Delta Dental PPO dentist, Delta Dental Premier dentist, or out-of-network (non-participating) dentist. Locate a Delta Dental network provider at deltadentalva.com.
- Preventive exams do not apply toward your annual maximum benefit.
- You will pay less out of your pocket when you see a Delta Dental PPO dentist.
- Delta Dental PPO and Premier dentists file claims directly with Delta Dental and accept Delta Dental’s reimbursement in full for covered services. When you see a PPO or Premier dentist, you will only be responsible for your deductible and coinsurance for covered services. Non-covered services are subject to balance billing.
- If you choose to see an out-of-network dentist, you will incur additional out-of-pocket expenses, and you will be billed the total amount the dentist charges (balance billing).
- When you see a Delta Dental PPO or Premier dentist, you are protected from balance billing for covered services.
The table below summarizes key features of the dental plan. The coinsurance amounts listed reflect the amount you pay. Please refer to the official plan documents for additional information on coverage and exclusions.
Regular dental visits tell your dentist a lot about your overall health, including whether or not you may be developing a disease like diabetes, heart disease, kidney disease, and some forms of cancer.
MAXOVER
The MaxOver benefit allows you to carry forward a portion ($375) of your unused annual benefit maximum for use in future years. In order to be eligible, you must have at least one preventive exam and cleaning during the year and your claims must be less than the $750 MaxOver claims limit paid during the year.
NEW!—SPECIAL HEALTH CARE NEEDS BENEFIT
Specifically for our members with special health care needs who may be eligible for additional services including exams, hygiene visits, dental case management, and sedation/anesthesia. Special health care needs include any physical, developmental, mental, sensory, behavioral, cognitive, or emotional impairment or limiting condition that requires medical management, health care intervention, and/or use of specialized services or programs. The condition may be congenital, developmental, or acquired through disease, trauma, or environmental cause and may impose limitations in performing daily self-maintenance activities or substantial limitations in major life activity.
Eligible members should let their dentist know that their Delta Dental group plan includes the special health care needs benefit and that they have a qualifying need.
- Extra exam benefits are included for additional consultations with the dentist that may be necessary to help patients understand what to expect prior to treatment.
- Up to four dental cleanings in a benefit year.
- Treatment delivery modifications, including anesthesia, necessary for dental staff to provide oral health care for patients with sensory sensitivities, behavioral challenges, severe anxiety, or other barriers to treatment.
DENTAL COSTS
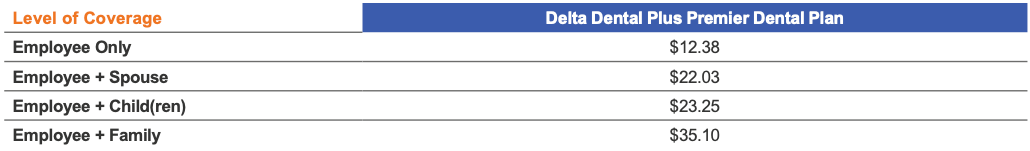
Listed below are the per-pay-period (26 pay periods per year) deductions (costs) for dental insurance. The amount you pay for coverage is deducted from your paycheck on a pre-tax basis, which means you don’t pay taxes on the amount you pay for coverage.